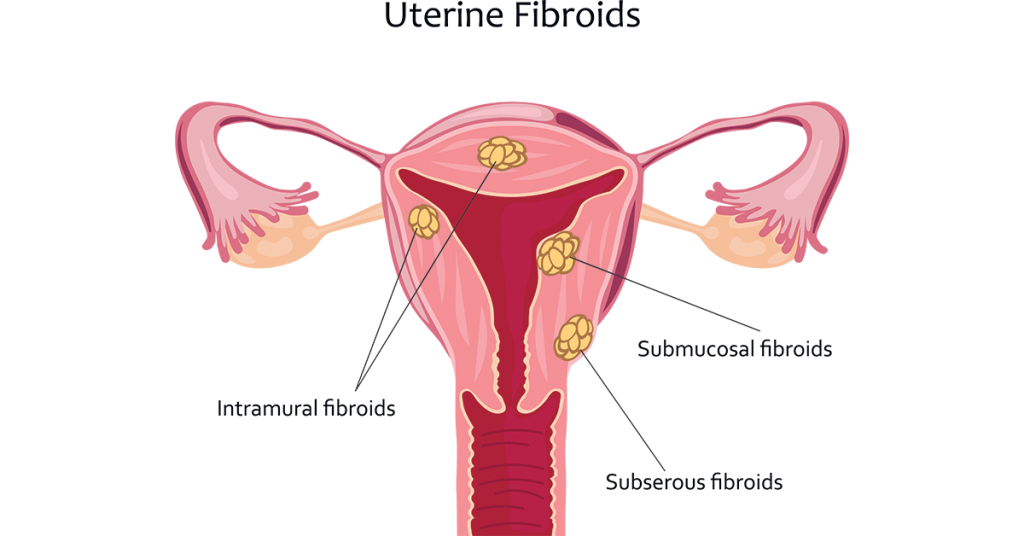
A fibroid, also known as uterine fibroid or leiomyoma, is a non-cancerous growth of the uterus (womb). These growths are made up of muscle and fibrous tissue and can vary in size. While many women with fibroids may not experience any symptoms, others may have symptoms like heavy menstrual bleeding, pelvic pain or pressure, and frequent urination. Fibroids can be diagnosed through various imaging techniques and are typically managed through medication or surgery, depending on their size and the severity of symptoms.
Reason for fibroid uterus :
The exact cause of uterine fibroids is not fully understood, but several factors may contribute to their development:
- Hormones: Hormones like estrogen and progesterone, which regulate the menstrual cycle and pregnancy, can stimulate the growth of fibroids. They tend to grow during the reproductive years when hormone levels are higher.
- Genetics: There appears to be a genetic component to fibroids, as they often run in families. If your mother or sister has fibroids, you may be at a higher risk.
- Hormone Replacement Therapy (HRT): Women who undergo hormone replacement therapy for menopausal symptoms may have an increased risk of developing fibroids, as these treatments often contain estrogen.
- Ethnicity: Some studies have suggested that certain ethnic groups, particularly African-American women, may have a higher risk of developing fibroids.
- Other factors: Obesity and a diet high in red meat and low in fruits and vegetables may also be associated with an increased risk of fibroids.
It’s important to note that while these factors may contribute to the development of fibroids, the precise cause can vary from person to person, and many women with risk factors never develop fibroids. Additionally, fibroids are non-cancerous and usually benign. If you suspect you have fibroids or have symptoms, it’s essential to consult with a healthcare professional for diagnosis and treatment options.
Why there is increase in fibroid uterus in young girls :
The increase in fibroid cases among young girls could be influenced by several factors, although research on this specific trend may be limited due to the relatively uncommon occurrence of fibroids in girls before they reach reproductive age. Some possible factors contributing to this increase could include:
- Obesity: The rising prevalence of obesity among children and adolescents is a concern. Obesity is associated with an increased risk of fibroids, so an increase in obesity rates could contribute to the rise in fibroids among young girls.
- Diet and Lifestyle: Unhealthy diets high in processed foods and low in fruits and vegetables, coupled with a sedentary lifestyle, can contribute to hormonal imbalances and obesity, both of which may be linked to fibroid development.
- Early Puberty: Girls are entering puberty at earlier ages in some cases. Early puberty can lead to longer exposure to the hormones estrogen and progesterone, which can influence fibroid growth.
- Environmental Factors: There is ongoing research into the potential role of environmental factors, such as exposure to endocrine-disrupting chemicals, in the development of fibroids.
- Genetic Factors: Genetic predisposition can play a role in the development of fibroids. If there’s a family history of fibroids, young girls may be at a higher risk.
It’s important to note that while fibroids can occur in young girls, they are still relatively rare in this age group. If a young girl experiences symptoms such as pelvic pain or heavy menstrual bleeding, it’s crucial for her to see a healthcare provider for a proper diagnosis and guidance on appropriate treatment options. Early detection and management can help mitigate the impact of fibroids on a young girl’s health and well-being.
Is there any risk factors for fibroid :
Yes, there are several risk factors associated with the development of uterine fibroids. These risk factors include:
- Age: Fibroids are most common in women of reproductive age, typically between the late 30s and early 50s. They tend to shrink after menopause when hormone levels decline.
- Family History: If your mother, sister, or close female relative has had fibroids, you may have an increased risk of developing them.
- Ethnicity: Some ethnic groups, particularly African-American women, have a higher risk of developing fibroids. They tend to develop them at a younger age and have more severe symptoms.
- Hormonal Factors: Estrogen and progesterone, two hormones that regulate the menstrual cycle, can promote the growth of fibroids. Hormonal imbalances or hormone replacement therapy (HRT) may increase the risk.
- Obesity: Being overweight or obese is associated with an increased risk of fibroids. Fat cells can produce excess estrogen, which may stimulate fibroid growth.
- Diet: A diet high in red meat and low in fruits and vegetables may increase the risk of fibroids.
- Childbearing History: Women who have not given birth or had their first child at an older age may be at a higher risk.
- Early Menstruation: Starting menstruation at an early age (before 10 years old) may increase the risk of fibroids.
- Lifestyle Factors: Sedentary lifestyles, lack of physical activity, and high-stress levels have been associated with a higher risk of fibroids in some studies.
- Environmental Factors: Some research suggests that exposure to certain environmental toxins and endocrine-disrupting chemicals may contribute to fibroid development.
It’s important to remember that having one or more of these risk factors doesn’t guarantee that you’ll develop fibroids, and many women with risk factors never experience them. If you have concerns about fibroids or are experiencing symptoms, consult with a healthcare provider for proper evaluation and guidance. Early detection and management can help address any potential issues related to fibroids.
Investigations :
When investigating uterine fibroids or suspected fibroids, healthcare providers may use a combination of the following diagnostic and investigative methods:
- Physical Examination: The doctor will perform a pelvic examination to check for the presence and size of fibroids. This is often the initial step in diagnosis.
- Ultrasound: Transvaginal or abdominal ultrasound is a common and non-invasive imaging method used to visualize the uterus and detect the size, number, and location of fibroids.
- MRI (Magnetic Resonance Imaging): MRI provides detailed images of the uterus and can help determine the size, location, and characteristics of fibroids. It’s especially useful for assessing large or complex fibroids.
- Hysterosalpingography: This involves injecting a contrast material into the uterus and taking X-ray images to evaluate the uterine cavity and fallopian tubes. It can help detect submucosal fibroids that protrude into the uterine cavity.
- Hysteroscopy: A thin, lighted tube (hysteroscope) is inserted through the cervix into the uterus to directly view the uterine cavity. This is useful for identifying and often treating submucosal fibroids.
- Endometrial Biopsy: In cases of abnormal bleeding, a sample of the uterine lining may be taken for analysis to rule out other causes and confirm the presence of fibroids.
- Blood Tests: Blood tests may be conducted to measure hormone levels (such as estrogen and progesterone) to assess their influence on fibroid growth.
- Laparoscopy: In some cases, a laparoscopic procedure may be performed to view the outside of the uterus and surrounding organs, helping to detect fibroids and assess their impact.
- Biopsy: If there is suspicion of cancer or if the fibroids exhibit unusual characteristics, a biopsy may be performed to collect a tissue sample for further analysis.
The choice of investigative methods depends on the patient’s symptoms, medical history, and the healthcare provider’s clinical judgment. Once fibroids are diagnosed, the healthcare team can discuss treatment options, which may include medication, minimally invasive procedures, or surgery, depending on the severity of symptoms and the patient’s preferences.
Treatment :
The treatment for uterine fibroids depends on various factors, including the size and location of the fibroids, the severity of symptoms, the patient’s age, and their desire for future fertility. Here are some common treatment options:
- Watchful Waiting: If fibroids are small and not causing significant symptoms, a doctor may recommend monitoring the condition without immediate intervention. This is often the case for women who are nearing menopause when fibroids typically shrink.
- Medications:
- Pain Relievers: Over-the-counter or prescription pain relievers can help manage pain and discomfort caused by fibroids.
- Hormonal Therapy: Medications like birth control pills, progestin-releasing IUDs, or GnRH agonists may be used to regulate heavy bleeding and reduce the size of fibroids.
- Tranexamic Acid: This medication can help reduce heavy menstrual bleeding.
- Minimally Invasive Procedures:
- Uterine Artery Embolization (UAE): This procedure blocks the blood supply to the fibroids, causing them to shrink. It’s a minimally invasive alternative to surgery.
- Myomectomy: A surgical procedure to remove fibroids while preserving the uterus. This can be done laparoscopically or through open surgery, depending on the size and location of the fibroids.
- Hysteroscopic Myomectomy: Used for submucosal fibroids, this procedure involves removing fibroids through the cervix using a hysteroscope.
- Surgical Options:
- Hysterectomy: A surgical procedure to remove the uterus. It is a definitive treatment for fibroids but ends fertility.
- Endometrial Ablation: This procedure destroys the uterine lining and is primarily used to treat heavy menstrual bleeding caused by fibroids.
- Focused Ultrasound Surgery: Magnetic Resonance-guided High-Intensity Focused Ultrasound (MRgFUS) is a non-invasive technique that uses ultrasound waves to heat and destroy fibroid tissue.
- Traditional Surgery: In some cases, particularly when fibroids are very large or numerous, traditional open surgery (laparotomy) may be required.
- Lifestyle Changes: Maintaining a healthy lifestyle, including regular exercise and a balanced diet, can help manage fibroid symptoms and prevent their growth.
The choice of treatment depends on the individual’s specific circumstances and preferences. It’s important to have a thorough discussion with a healthcare provider to determine the most appropriate treatment plan. Treatment can alleviate symptoms, improve quality of life, and, in some cases, preserve fertility.
Pinpoint precautions :
Certainly, here are some specific precautions and lifestyle changes that can help manage and prevent complications related to uterine fibroids:
- Regular Check-ups: Schedule regular visits with your healthcare provider to monitor the size and growth of fibroids and discuss any changes in symptoms.
- Pain Management: If you experience pain or discomfort due to fibroids, work with your healthcare provider to develop a pain management plan. Over-the-counter pain relievers or prescription medications may be recommended.
- Healthy Diet: Aim for a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Some research suggests that a diet high in fiber and low in red meat may help reduce the risk of fibroids.
- Maintain a Healthy Weight: Obesity is associated with an increased risk of fibroids. Maintaining a healthy weight through regular exercise and a balanced diet can be beneficial.
- Exercise Regularly: Regular physical activity can help reduce the risk of fibroids and alleviate symptoms. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Stress Management: Chronic stress may contribute to hormonal imbalances that can affect fibroid growth. Practice stress-reduction techniques such as yoga, meditation, or deep breathing exercises.
- Limit Alcohol and Caffeine: Excessive alcohol and caffeine consumption may be associated with a higher risk of fibroids. Limit your intake of these substances.
- Stay Hydrated: Drinking plenty of water can help reduce bloating and alleviate some fibroid symptoms.
- Avoid Smoking: Smoking has been linked to an increased risk of fibroids and can worsen symptoms.
- Birth Control: Discuss birth control options with your healthcare provider. Some forms of birth control, like hormonal IUDs or birth control pills, may help manage fibroid-related bleeding and pain.
- Pregnancy Planning: If you plan to have children and have fibroids, consult with a healthcare provider to discuss how fibroids might affect fertility and pregnancy. In some cases, myomectomy (fibroid removal) may be an option to preserve fertility.
- Regular Menstrual Care: Keep track of your menstrual cycles and report any changes or irregularities to your healthcare provider.
- Educate Yourself: Understand your condition and the available treatment options. This will help you make informed decisions about your healthcare.
Remember that these precautions can help manage fibroid symptoms and reduce the risk of complications. It’s essential to consult with a healthcare provider for personalized advice and treatment options tailored to your specific situation.Post navigation